From a young age, I’ve always loved reading and writing. They seem to fit much better in my brain than numbers. Over the years, particularly working in education roles, I’ve come to appreciate that words hold immense power in healthcare. They shape our identity, practice, and even how care is delivered (or should I say, provided—but more on that shortly!).
Residents, Clients, Consumers… Now ‘Individuals’
A recent shift in language made me stop and reflect on just how much words matter.
Just announced this week, the Aged Care Act 2024 and strengthened Aged Care Quality Standards will refer to the older person as the individual. This tightening of language reinforces person-centred care and ensures that terminology aligns with evolving regulatory expectations.
It reminded me of two other key moments in my career where a simple change in phrasing transformed the way I think about nursing, aged care, and even the people we care for.
Nurses Provide Care - We Do Not Deliver It
The first example is one I feel so strongly about that I correct it every chance I get, whether in articles, consultation submissions, or everyday conversations.
It all goes back to a session I attended in the U.S. about a decade ago. Back then, I was lucky enough to travel regularly to the National Nurse Practitioner Symposium in Colorado as part of my role at Ausmed. These trips were invaluable, giving us access to the latest clinical updates that shaped our conferences and content for an entire year.
But one session, in particular, changed my perspective forever.
Marlene Kramer, a name many in nursing education will recognise, spoke about reality shock in nursing and why nurses leave nursing. In this particular conference session, she explored the challenges new graduates and novice nurses face, especially when juggling multiple complex patients, and how these pressures conflict with nursing's holistic identity.
And then she said something that stuck with me ever since:
“Nurses do not deliver care. We provide it.”
The difference is subtle, but the impact is profound.
Taxis (or Ubers, now) deliver people. Supermarkets deliver groceries. Healthcare isn’t about dropping off a product. It’s about providing holistic, person-centred care that recognises the whole individual. Yes we have to-do lists and things must get done. But there are real dangers in seeing nursing (and healthcare) as task-orientated jobs. They are so much more than that.
That distinction matters. It’s why, to this day, I continue to edit, correct, and advocate for the use of “provide” rather than “deliver.” Words shape identity, and as nurses, our identity must always be grounded in holism, critical thinking, and genuine human connection.
Nursing Homes Were Once Run by Nurses
Just writing Nursing Home in that sub-title seems strange and shows how far we’ve strayed.
This second example reflects on history, not so much my career, but it’s incredibly relevant today. Before Ausmed became what it is now, we were a publishing company. Our first-ever book?
Care of the Person with Urinary Incontinence.
And one of the first conferences we ran? Nursing Home Nurses. Ironically, ran when the standards first came out in the early 1990s.
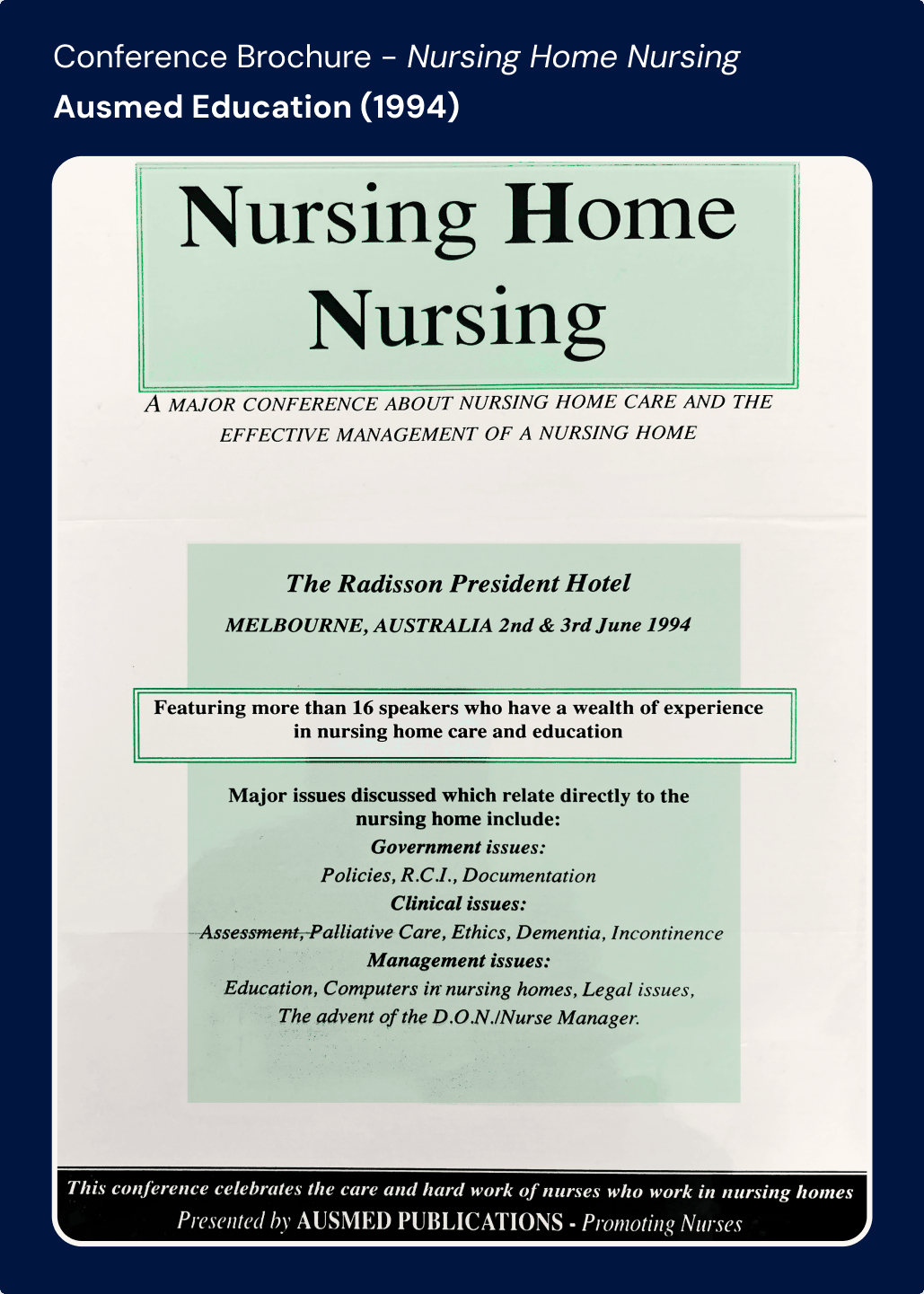
I’m deliberately using the phrase "nursing home" here because that’s exactly what they were. That’s what we called them. And most importantly, that’s who ran them - nurses.
Fast-forward to today, and we’ve swung wildly in the other direction. Over the years, we have moved away from “nursing homes” and towards “residential aged care facilities.”
At the same time, we removed nurses from these settings, replacing them with broader care teams.
And now? The pendulum is swinging back.
With mandatory care minutes reintroducing nurses into aged care, we’re correcting an imbalance. But it’s a fascinating case study of how language reflects systemic shifts. We changed what we called these facilities, and gradually, we changed the entire model of care.
Words matter. And in aged care, the words we choose often predict the policies we follow.
‘Individuals’ - The Newest Change
This third and most recent example is one of the most recent and intriguing changes in healthcare language.
As mentioned above, this week, it was shared that in the Aged Care Act 2024 and the strengthened Aged Care Quality Standards that we will no longer refer to older people in residential care as residents, clients, or consumers. Instead, they are simply individuals.
It’s a fascinating linguistic choice.
For years, we moved towards calling people in care “consumers” and “clients” - a reflection of the broader consumer-directed care movement. It was about putting choice and control into the hands of those receiving care, and I absolutely agree with that intent.
But this new shift to “individuals” feels different.
It strips away labels that might impose a transactional or institutional identity. It removes a whiff of ageism. It refocuses on personhood, ensuring that people in care are not just recipients of services but unique individuals with their own needs, preferences, and identities.
This weekend, my family is about to celebrate my Dad’s 80th Birthday. He planks for 11 minutes daily, rides his bike, often up to 10km per day and is an incredibly active contributor to society. He is lucky enough to have his health, live happily at home, and not feel like an Octogenarian. But - should that change, or for friends and family that are receiving care, this shift gives me hope that they too would be seen for who they are, not their age or list of past medical conditions that sit on their (hopefully, electronic) medical record. That’s another change for another article.
I love this change because it subtly but powerfully brings holism back into the conversation, a full-circle moment in how we define care.
Words Shape the Way We Care
These three moments in my career have cemented my belief that the words we use aren’t just semantics. They shape identity, policy, and practice.
- We do not deliver care, we provide it. Because healthcare is holistic.
- Nursing homes were run by nurses — until we changed the language. Now, we’re bringing them back. Surprise, surprise.
- The Aged Care Act 2024 calls people in care “individuals.” A simple but powerful shift towards dignity and person-centeredness.
Practically speaking, this means we will now actively encourage and support others in updating terminology across both written and video content.
For a provider and large publisher of education like Ausmed, this is a huge undertaking—we have an extensive library of resources and thousands of pages on our website. Of course, there will be times when you see, read, or hear the previous terminology simply due to the sheer volume of content.
But we are committed to making this change wherever we can. Because words don’t just describe reality. They shape it.
And that’s why I’ll always be an advocate for choosing them wisely.
Ensure your organisation is prepared for your first audit under the strengthened Standards.
Author
Zoe Youl
Zoe Youl is a Critical Care Registered Nurse with over ten years of experience at Ausmed, currently as Head of Community. With expertise in critical care nursing, clinical governance, education and nursing professional development, she has built an in-depth understanding of the educational and regulatory needs of the Australian healthcare sector.
As the Accredited Provider Program Director (AP-PD) of the Ausmed Education Learning Centre, she maintains and applies accreditation frameworks in software and education. In 2024, Zoe led the Ausmed Education Learning Centre to achieve Accreditation with Distinction for the fourth consecutive cycle with the American Nurses Credentialing Center’s (ANCC) Commission on Accreditation. The AELC is the only Australian provider of nursing continuing professional development to receive this prestigious recognition.
Zoe holds a Master's in Nursing Management and Leadership, and her professional interests focus on evaluating the translation of continuing professional development into practice to improve learner and healthcare consumer outcomes. From 2019-2022, Zoe provided an international perspective to the workgroup established to publish the fourth edition of Nursing Professional Development Scope & Standards of Practice. Zoe was invited to be a peer reviewer for the 6th edition of the Core Curriculum for Nursing Professional Development.



