Improvements in Acquiring New Nurses
We have all heard projections that there will be a shortfall in the nursing workforce within Australia and globally. Significant efforts to recruit more nursing undergraduates into programs are well underway. Alongside this, our governing body, the Australian Health Practitioner Regulation Agency (Ahpra), and the National Boards are removing burdensome restrictions, allowing recognition of more international nursing qualifications within Australia.
According to the Ahpra annual report: Growing a safe workforce, in 2022/23, there was a 2.1% increase in the registration of nurses and midwives; this included approximately one-third of all newly registered nurses originating from overseas (Ahpra, 2022/23).
The efforts to attract more nurses are working. So, I want to talk about what our newly registered nurses face next and the challenge of keeping them in the profession they have spent the last two or more years working towards.
The Real Issue is Retention
Dropout rates in the first 12 months of graduate nurses in Australia range from 2-8%, with reported intention to leave the profession as high as 20%. So we have a problem!
I am a proud nurse of nearly 20 years. I entered this profession with a passion for helping people in a crisis. My focus was always on acute hospital care. I understood that nursing could take me places around the country and the world if that’s what I desired. I achieved good grades in high school, which opened up almost any career I could pursue. I chose nursing.
My university experience fostered further passion, instilling in me a pride for my profession and an expectation of critical thinking, questioning, and providing holistic care to my future patients, their loved ones, and the community.
I completed my final year and left with the fears that many graduates still feel today:
- Am I prepared to care for 4-5 patients?
- Am I safe?
- Am I equipped to deal with death and grief?
It’s for these reasons and more that I chose to apply for a graduate program.
Transition to Practice Programs
Graduate programs promote themselves as providing structure, support, and dedicated people within an organisation who understand that I am a novice nurse and will have different needs. Graduate programs offer some reassurance to novice nurses that a workplace will have different expectations of them.
These desires are as true today as they were then. I’ve staffed booths at nursing expos, presented to groups of students, and worked closely with undergraduate students, and they all share the same concerns I had all those years ago.
Are these fears becoming a reality that are driving people to leave the profession so soon?
What Do Nurses Want?
The literature sheds some light on the situation. However, as so many of these studies have low numbers of participants who leave the profession in their first 12 months and are qualitative, we are collecting data on self-reflection from people under stress.
We hear that Generation Z nurses are different. I would dispute this overly basic assumption. All people want similar things from any career: recognition, opportunity, and autonomy. What makes nursing different is the degree of workplace stress we expect nurses to deal with as just “part of the job”.
Studies also tell us that interactions with front-line leaders significantly affect people's ultimate decision to leave the workforce.
For this reason, many organisations worldwide are developing frontline nursing leader programs to better equip nursing managers with the skills to support their staff, develop their staff, and have difficult conversations. This literature informs much of the work of our national nursing workforce strategy.
Essentially, nurses want greater recognition, greater autonomy, and greater opportunity.

1. Greater Recognition
We can’t deny that recognition must include decent pay that reflects the nurses' work. I won’t begin a diatribe about nursing pay or the starting wage for a graduate nurse only to say we deserve better!
Recognition for a graduate speaks more to their frontline managers and colleagues who support them when faced with the challenges of nursing that we all know exist. Adjusting to a new profession like nursing can be stressful. That’s why so many graduate programs now front-load support at the beginning of the year or at rotations and slowly taper down.
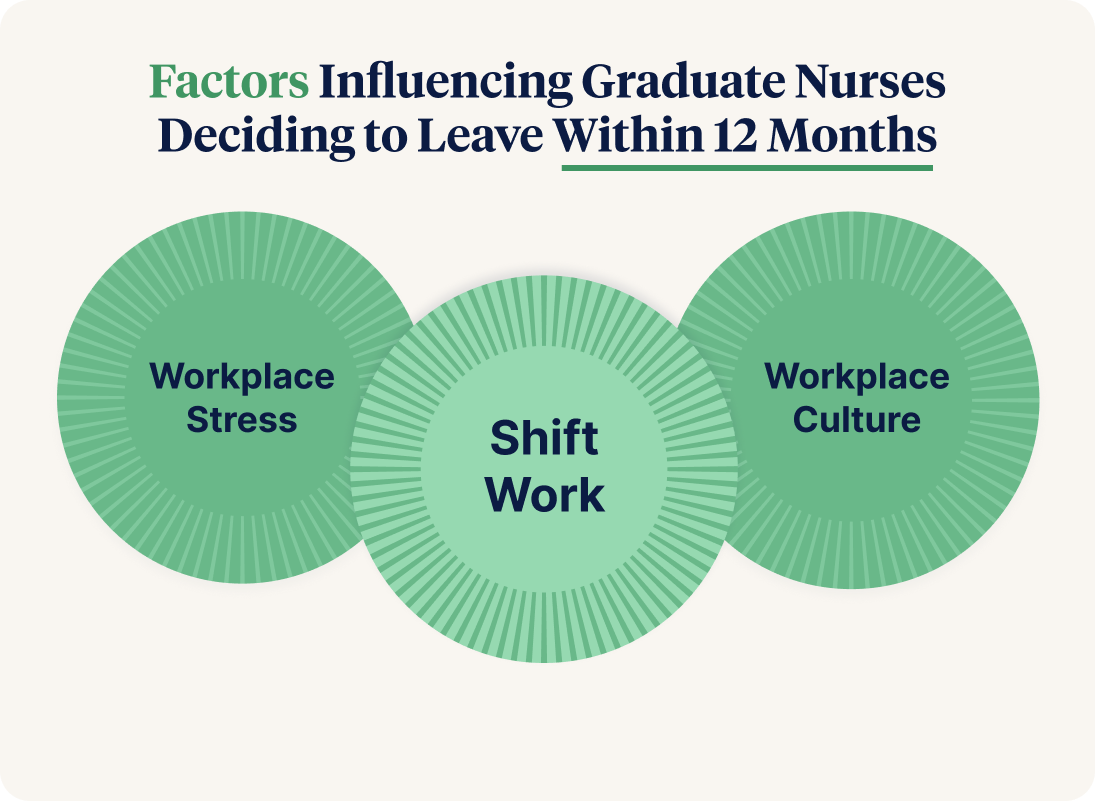
However, clinical support is not the main reason people leave within the first 12 months. Although graduates tell us they want clinical support when heading into their careers, other factors ultimately significantly influence the intention to leave within the first 12 months.
Shift work
24/7 shift work is hard, especially if you have other roles within your family and community that conflict with those working hours. Society now expects workplaces to recognise the need to disconnect and have better work-life balance. We accept healthcare as a 24/7 service, but approaching conversations about the challenges of shift work and weekend work with genuine understanding will help. We need to advocate for genuine work-life balance for shift workers.
This can be as simple as asking yourself if a staff member's request to not work one day or one shift because of a commitment in other parts of their life is unreasonable. Imagine how respected and seen that nurse will feel if they are met with compassion.
Workplace stress
Negative interactions with colleagues, nursing, medical or other, and patients and their loved ones significantly impact our early career nurses. They can set the tone for the months ahead. We know that a healthier workplace culture improves patient outcomes.
These negative interactions are amplified when they happen to graduate nurses. They tell us this with their survey results with an intention to stay in a clinical area or profession. We also understand that all junior healthcare workers feel underprepared to deal with death, dying, acute mental health crises, and patients under the influence of drugs. How could they be prepared?
These are extreme situations for anyone to deal with. Immediate follow-up from a senior nursing colleague following significant clinical incidents is crucial to building rapport, demonstrating recognition and understanding, and fostering an open dialogue between the nurse and their manager so that interactions are not limited to when things go wrong.
Workplace culture
Respect from colleagues speaks to the fact that these are qualified nurses. Too often, graduates are dismissed as the “grad.” Workplace culture is set by workplace managers. We must find ways to integrate early-career nurses into teams as soon as possible. That doesn’t have to be in the immediate clinical area; there are other ways to foster a sense of belonging in an organisation.
2. Greater Autonomy
Scope of Practice
Lately, there has been discussion about nurses needing to work to the upper limit of their scope of practice to achieve greater job satisfaction and improve retention. I passionately agree and want to see senior nursing role models working at the upper limit of their scope to motivate and excite them to achieve their best.
However, I don’t think this is accurate for our graduate nurses; they must work comfortably within their scope of practice as they find their professional identity.
Rostering
Building upon what has been said earlier, we expect our new nurses to conform to the workplace instead of the workplace working with the individual. Too often, we do not fully respect that people have a life outside of work.
I think of my own example with night shift. I always slept poorly on the night shift. Eventually, I approached the nurse in charge of rostering and discussed one night per week every Sunday. I was fortunate that Sunday night was the most challenging shift to fill, and it worked with my sporting interests on a Sunday afternoon. I kept that arrangement for approximately six years.
We may be surprised that the requests of our early career nurses benefit both parties. But if an individual's request cannot be accommodated, provide a justification. It’s about valuing each individual as part of a team.
3. Greater Opportunity
Third on the list of ‘What Graduates Want’ are options. Opportunity brings together much of the above. If we engage with our graduate nurses early in their careers, we can help them explore the vast opportunities that nursing offers. This could mean career coaching on the steps needed to achieve the level of skill and competence of their senior colleagues working at a higher scope of practice or having clear discussions about what career they want for themselves over the next year or two.
Fortunately, nursing is a varied profession that is evolving rapidly in Australia to meet growing community needs. We must discuss the best career option for the individual early career nurse. It may not be in a ward. It might be in the operating theatre, an outpatient clinic, or the community, which begs the question: Are we set up to facilitate easy transitions from acute to subacute to community or residential aged care nursing?
We don’t want our latest professionals to leave the profession they had a passion for all those years ago when they signed up for their nursing degree just because their next step is unclear or seemingly out of reach.
Conclusion
My main point is that our early interactions with graduate nurses matter. Graduate nurses want recognition, autonomy and opportunities to transition to the next phase of their careers. Above all else, though, we must show passion and compassion and inspire the next generation to keep propelling our profession forward and ensure our communities get the best care possible.
“To do what nobody else will do, a way that nobody else can do, despite all we go through: that is to be a nurse.” - Rawsi Williams.
Read more about the issue of nurse retention rates and how a decline in the experience of the workforce can lead to incremental decline.
Related Resources
- Incremental Decline - The Road to Non-Compliance?
- Guide to Empowering Learners to Imrpove Compliance
- Guide to Navigating Compliance Chaos
- Guide to Mandatory Training
- A Guide for Managers: Mandatory Training in Aged Care
- Guide to Induction Training
- Induction Training - FAQs
- A Guide to Policy Management
- Creating an Education Framework
References
Australian Government Department of Health and Aged Care 2024., National Nursing Workforce Strategy, viewed 30 October 2024, https://www.health.gov.au/our-work/national-nursing-workforce-strategy.
Australian Government Department of Health and Aged Care 2024., Unleashing the Potential of our Health Workforce: Scope of practice review, viewed 30 October 2024, https://www.health.gov.au/our-work/scope-of-practice-review.
Australian Health Practitioner Regulation Agency (Ahpra) 2022/23, Annual Report: Growing a safe workforce 2022/23, Ahpra, viewed 30 October 2024, https://www.ahpra.gov.au/Publications/Annual-reports/Annual-report-2023.aspx.
Braithwaite, J., Herkes, J., Ludlow, K., et al. 2017, 'Association between organisational and workplace cultures and patient outcomes: systematic review', BMJ Open, vol. 7, e017708, https://doi.org/10.1136/bmjopen-2017-017708.
Fair Work Ombudsman n.d., Right to disconnect, viewed 30 October 2024, https://www.fairwork.gov.au/about-us/workplace-laws/legislation-changes/closing-loopholes/right-to-disconnect.
Jarden, R.J., Jarden, A., Weiland, T.J., Taylor, G., Bujalka, H., Brockenshire, N. & Gerdtz, M.F. 2021, 'New graduate nurse wellbeing, work wellbeing and mental health: A quantitative systematic review', International Journal of Nursing Studies, vol. 121, 103997, https://doi.org/10.1016/j.ijnurstu.2021.103997.
Madden, C. 2024, Gen Z Future Employability Skills, Claire Madden, viewed 13 November 2024, https://clairemadden.com/category/blog/gen-z-future-employability-skills.
Mazzetti, G. & Schaufeli, W.B. 2022, 'The impact of engaging leadership on employee engagement and team effectiveness: A longitudinal, multi-level study on the mediating role of personal- and team resources', PloS One, vol. 17, no. 6, e0269433, https://doi.org/10.1371/journal.pone.0269433.
Rabin, S., Kika, N., Lamb, D., Murphy, D., Am Stevelink, S., Williamson, V., Wessely, S. & Greenberg, N. 2023, 'Moral Injuries in Healthcare Workers: What Causes Them and What to Do About Them?', Journal of Healthcare Leadership, vol. 15, pp. 153–160, https://doi.org/10.2147/JHL.S396659.
Ramsay Health Care and Bupa n.d., Ramsay Health Care and Bupa join forces to develop our next generation of nurses, viewed 30 October 2024, https://media.bupa.com.au/ramsay-health-care-and-bupa-join-forces-to-develop-our-next-generation-of-nurses/.
Author
Tony King
Tony King is a registered nurse and intensive care nurse educator with Epworth Healthcare. He completed a research Masters by evaluating factors that influence quality end-of-life care. Tony is passionate about developing all healthcare professionals, recognising we all have knowledge and strengths that positively contribute to a patient's journey.



