Why Workforce Capability Resonates with Me
Over the past year, but particularly in the last month, I’ve had the privilege, as a senior leader at Ausmed Education, of being a part of one of the most significant changes in our company’s history. Ausmed was founded in 1987 (we will need to start planning our 40th birthday party soon), and having spent nearly 14 years at Ausmed, change isn’t new to me. We’re agile, always moving with the times - often ahead of them - so even just thinking about a shift feels natural.
I’ve seen firsthand how we’ve evolved from books to online publishing, from face-to-face events to online education, from creating a CPD App to developing a Workforce Capability System. And that’s the latest change I’m embracing and reflecting on the most right now.
We’ll talk a lot more about this in the coming months, and I won’t steal too much of the thunder from people like Will Egan, our CEO, who’s incredibly excited and proud of this new direction. But even our mission statement is evolving to reflect it. While improving care will always be at the heart of everything we do, there’s a shift in how we do that. We've long supported clinicians with their education, and more recently, particularly post-COVID, we’ve expanded into organisational learning and development.
We agreed on the right words just last week, and I’m proud to share that Ausmed’s mission is to improve healthcare by building workforce capability.
I’ve been reflecting on why this extension feels so right. The more I think about it, the more workforce capability just makes sense. Here are four that stand out.
1. Millers' Model of Clinical Competence
Why Knowledge Alone Isn’t Enough
Millers' Model of Clinical Competence was one of the first models I encountered outside of clinical concepts like wound care or infection control. Miller’s model fundamentally shaped how I think about education and professional development.
The model suggests that competence isn’t built through knowledge alone. Instead, learning must move through distinct stages: acquiring knowledge, developing a skill, putting that skill into practice, and ultimately demonstrating it with confidence and expertise.
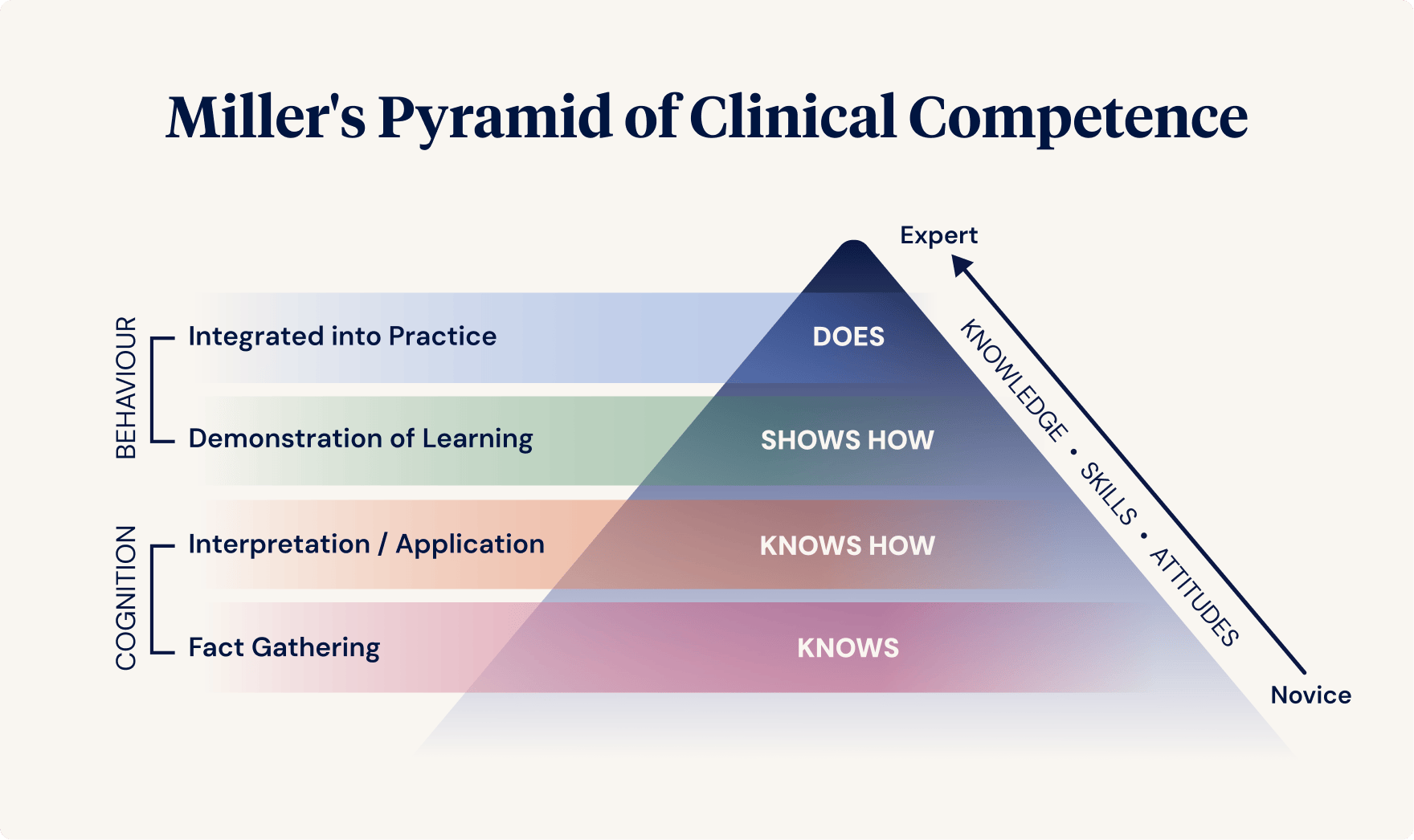
Providing healthcare can’t stop at knowledge. A person might know the correct steps for performing a clinical skill, but competence isn't reached until they can repeatedly demonstrate that skill with confidence, consistency, and in the context of everyday practice. Beyond that, how we perform the skill matters, too - our attitude, as part of a team and the broader communities in which we apply it.
This aligns so well with the shift to workforce capability. We can’t think about education, skills, attitudes, or competence in isolation because healthcare itself is holistic and person-centred. Why should the key concepts underpinning our practice be treated any differently?
2. The Shift From CNE to CPD
Moving from ‘Hours’ to Outcomes
I can’t remember the exact year, maybe around 2010, but I distinctly recall a shift in how we spoke about professional development in nursing.
The Ausmed Education Learning Centre’s accreditation with the American Nurses Credentialing Center (ANCC) has meant I’ve always built strong ties with the Association for Nursing Professional Development (ANPD), which is a peak body that represents nursing professional development (NPD) practitioners globally.
For years, we talked about CNE (Continuing Nursing Education) points and hours - tracking time spent learning, almost as if compliance was the primary goal. But then, the language started to change. We moved towards CPD (Continuing Professional Development), and it was more than just semantics.
The shift was about recognising that professional development isn’t just about accumulating hours; it’s about learning that impacts practice. Outcomes-based learning is the future. Actually, it's already here.
This was a crucial turning point.
We moved away from the idea of ‘ticking the box’ in education and instead focused on building real skills and competence, which aligns perfectly with the shift to workforce capability.
The shift also flowed through to job titles and recognised that the role of an Educator was not just to educate! As any educator (or however your title has changed over time) will tell you, it is so much more! “Educators” are change agents, leaders, project managers, mentors, and facilitators — just to name a few!
3. Education Isn’t Always the Solution (and That’s Okay)
This might be a surprising statement from someone who has spent years leading education at Ausmed. I genuinely love education! I always talk about it in webinars, articles, and podcasts (I literally cannot believe how much I spoke in a recent episode #cringe). But here’s the truth:
Education doesn’t solve every problem.
Too often, education is treated as a catch-all solution for workplace challenges. Educators (whatever the formal title) frequently bear the brunt of an organisation’s “wishlist” of problems to be solved. But many of these challenges aren’t actually education gaps at all.
Pam Dickerson, a beloved mentor and absolute powerhouse of NPD, taught me this very early on. A knowledge gap, validated with evidence, triggers a genuine need for an education initiative. But sometimes, dare I say, often, the real issue (or gap, to be precise) is:
- A missing or unclear policy
- A flawed system or process
- A governance or leadership issue
- A lack of available resources
- A nasty pastie (I am trying to say, a “people” issue!)
Simply rolling out more education (oh, and please, no) and making it mandatory does nothing to solve these kinds of problems. If the issue isn’t knowledge or skill-related, education just isn’t the answer.
That’s why I’m so comfortable embracing workforce capability. It acknowledges that education is just one tool that, when used wisely, is effective, but there’s a larger set of initiatives and approaches we can systematically leverage to improve practice and healthcare outcomes.
4. Measuring Impact - How Do We Know It’s Working?
This brings me to my final reflection, which ties back to my Master’s thesis I finished in 2020. My research focused on evaluating the impact of CPD, not just whether people were completing training, but how one might assess if it was making a real difference.
I was grappling with deeply personal questions at the time: If I step away from direct patient care and resign from ICU, will I still make a difference? Will I still be relevant? Am I still a nurse?
When I worked in intensive care, I could quantify my impact: If I worked three 12-hour shifts per week, looking after one patient daily, I would directly care for about 150 patients annually. Great! That really suits the ICU nurse personality way of thinking! I love it.
I can calculate it, just like I could calculate how much noradrenaline a post-op cardiothoracic patient needed when their blood pressure was falling through the floor (and calculate fluid requirements, just to show that, yes, I remember you can’t pump empty pipes!).
I digress. But moving into an education role at Ausmed, how would I know if I was making a difference? Another calculation got me over the line and excited me, and very soon, I was hooked.
I was writing 250–300+ conferences and seminars per year, each with high attendance. I was influencing tens of thousands of healthcare professionals, who, in turn, impacted vast numbers of people in our community.
That was incredibly powerful, but it wasn’t enough to assume it made a difference. That’s why I studied how we can measure the impact of CPD.
And what I found reinforced everything I’ve shared here.
If education stops at knowledge, it’s not enough.
If we don’t support learners to:
- Build skills
- Demonstrate competence
- Overcome barriers to translation (like forgetting it)
- Apply it in practice
- Bring the right attitude
- And measure it
- And measure (some initiatives) again, long after the activity was completed,
… then what’s the point?
This is precisely why workforce capability makes sense. It moves us beyond education and compliance and helps us ensure that learning isn’t just something people complete. We can’t just work towards someone feeling satisfied that the learning environment was lovely or that a learner got 10/10 multiple-choice questions correct. As Pam says, so what?
When capability-building activities are done systematically, we translate actions into impact, not just knowledge into practice.
Final Thoughts - It Just Makes Sense!
I’ve spent over a decade working in education and have seen how learning in healthcare has evolved. I know workforce capability is the right direction because it aligns with everything I’ve learned along the way.
It acknowledges that knowledge alone isn’t enough.
It focuses on real people’s careers, confidence and practice development, not just compliance.
It ensures education is used strategically — not as a one-size-fits-all fix.
Most importantly, it pushes us to measure impact so we know our work is making a difference.
This is an exciting time at Ausmed, and I couldn’t be prouder to be part of it.
Because improving healthcare has always been our mission. And now, we’re doing it by building workforce capability.
What’s Next?
Does this resonate with you? If you’re also thinking about the evolution from education to capability, I’d love to hear your thoughts. Feel free to email me at zoe@ausmed.com.au, join an upcoming webinar, or watch some previous ones here.
Author
Zoe Youl
Zoe Youl is a Critical Care Registered Nurse with over ten years of experience at Ausmed, currently as Head of Community. With expertise in critical care nursing, clinical governance, education and nursing professional development, she has built an in-depth understanding of the educational and regulatory needs of the Australian healthcare sector.
As the Accredited Provider Program Director (AP-PD) of the Ausmed Education Learning Centre, she maintains and applies accreditation frameworks in software and education. In 2024, Zoe lead the Ausmed Education Learning Centre to achieve Accreditation with Distinction for the fourth consecutive cycle with the American Nurses Credentialing Center’s (ANCC) Commission on Accreditation. The AELC is the only Australian provider of nursing continuing professional development to receive this prestigious recognition.
Zoe holds a Master's in Nursing Management and Leadership, and her professional interests focus on evaluating the translation of continuing professional development into practice to improve learner and healthcare consumer outcomes. From 2019-2022, Zoe provided an international perspective to the workgroup established to publish the fourth edition of Nursing Professional Development Scope & Standards of Practice. Zoe was invited to be a peer reviewer for the 6th edition of the Core Curriculum for Nursing Professional Development.



