Aged care is fundamentally about people—the older people who depend on care, services, and the workforce that provides them. A capable, well-supported workforce is essential for providing consistent, safe, high-quality care. Without a strong workforce, care quality suffers, organisational risks increase, and staff experience burnout or dissatisfaction.
Outcome 2.8 of the strengthened Aged Care Quality Standards focuses on ensuring that providers effectively plan for and manage their workforce to meet current and future care needs while fostering a safe and supportive environment for staff.
Understanding the Requirements
Outcome 2.8 sits within Standard 2, The Organisation. The placement of these requirements emphasises the organisation’s governing body (Board) accountability for establishing systems that support workforce development.
Specifically, the outcome the Commission is seeking within 2.8 is that “the provider understands and manages its workforce needs and plans for the future”, as demonstrated by two key actions on workforce planning and psychological safety.
Action 2.8.1: Workforce planning
The provider implements a workforce strategy to:
- Identify, record and monitor the number and mix of workers required and engaged to manage and deliver quality care and services.
- Meet minimum care requirements and engage with workers on how planning and rostering will achieve these requirements.
- Identify the skills, qualifications and competencies required for each role.
- Engage suitably qualified and competent workers.
- Use direct employment to engage workers whenever possible and minimise the use of independent contractors.
- Mitigate the risk and impact of workforce shortages and worker absences or vacancies.
Action 2.8.2: Psychosocial safety
The provider implements strategies for supporting and maintaining a satisfied and psychologically safe workforce.
Two Key Areas of Focus
Based on two key documents, Draft: Evidence Mapping Framework and The Strengthened Standards Provider Guidance material, we’ve summarised the key areas to prioritise to meet this requirement: creating a workforce strategy and prioritising the safety and wellbeing of their staff.
Within these two broad areas of focus are clear opportunities to review:
- How the organisation prioritises direct employment over contingent labour (use of agency staff, subcontractors, etc.).
- Contingency plans to manage workforce shortages or absences.
- Creating a culture of support and inclusion to aid workforce satisfaction.
- Systems to actively engage with their staff, through feedback.
- Opportunities for growth and development to build a resilient, motivated workforce.
Specific Actions
To meet the requirements of Outcome 2.8, providers can take the following steps:
- Develop a workforce strategy.
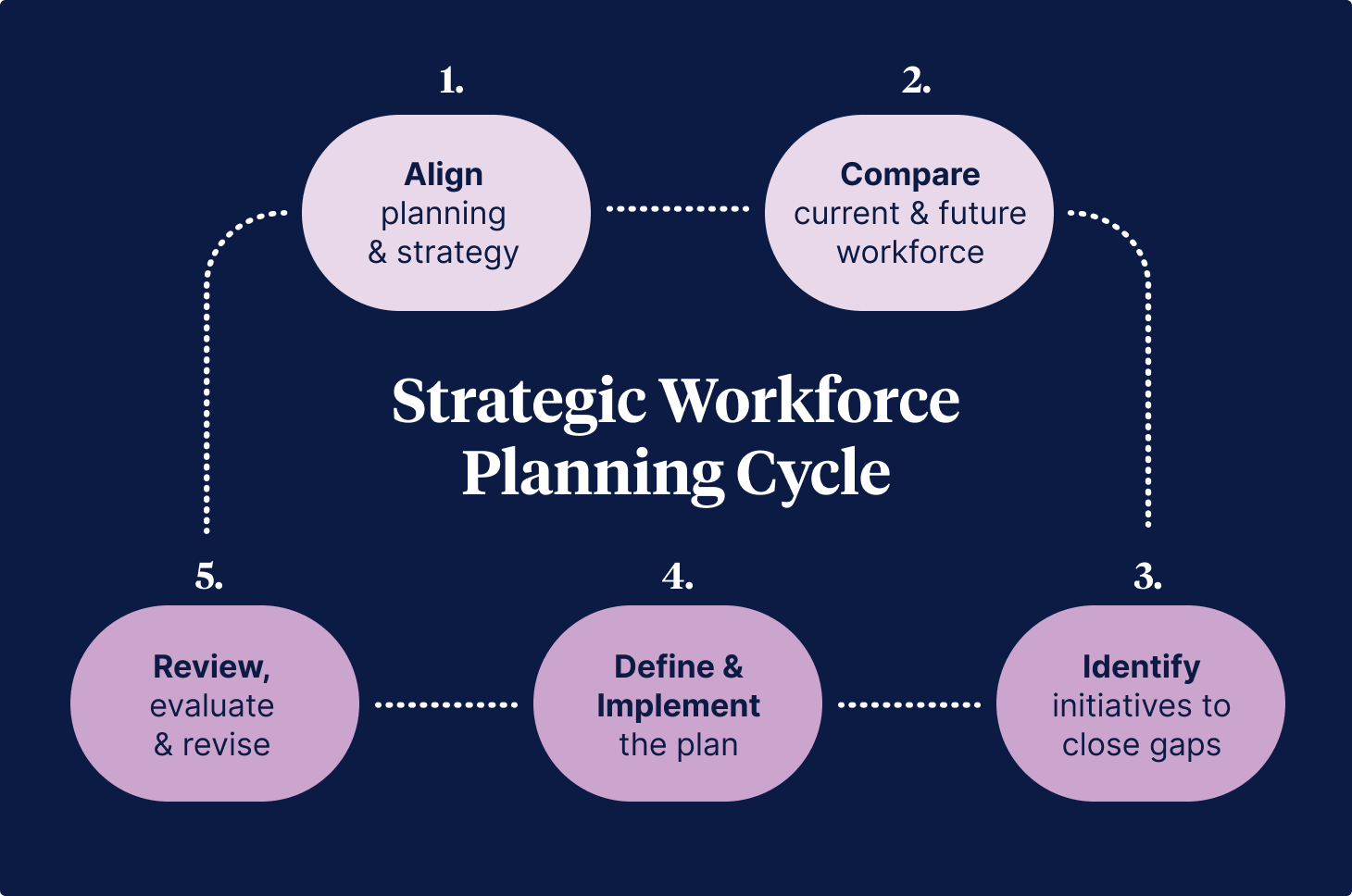
- Use a strategic workforce planning cycle to identify current and projected gaps in workforce skills and numbers.
- Establish or review the process to assess a worker’s qualifications, experience, skills, and suitability for the role before hiring them.
- Establish clear training strategies for staff development, including an effective training system (Outcome 2.9)
- Ensure competency-based education on core matters (at a minimum) is in place (Outcome 2.9)
- Review rostering practices to ensure they align with the organisation’s workforce strategy.
- Demonstrate a process is in place that strives to achieve the right skill mix
- Create mechanisms to connect staff performance goals with ongoing learning (Outcome 2.9)
- Implement workplace initiatives prioritising wellbeing and a psychologically safe and supportive work environment for all.
Creating a Workforce Strategy
Under Outcome 2.8 of the strengthened aged care quality standards, providers must establish and maintain a workforce planning strategy to meet care recipients' needs while supporting their workforce.
Developing a workforce strategy is a collaborative effort that involves various parts of the organisation and is supported (or sponsored) by senior leadership. By prioritising talent management, diversity, and adaptability to change, a workforce strategy offers forecasts and action plans to address future workforce needs while steering clear of excessive detail or short-term focus. To ensure its relevance and effectiveness, the strategy must be grounded in data and evidence tailored to the organisation's specific context.
The Guide to Workforce Strategy provides a detailed overview of how to create a workforce strategy within a structured workforce planning cycle.
Monitoring Workforce Strategy
Ongoing monitoring is essential to evaluate the effectiveness of the workforce strategy. Providers should establish key performance indicators (KPIs) to measure outcomes, regularly review progress, and adapt the strategy as necessary. Workforce data should be collected and analysed to inform decision-making and ensure alignment with care requirements.
Challenges Providers May Face
Workforce planning in aged care is not without its challenges. One of the most significant barriers is a lack of reliable workforce data. Without accurate data, it becomes difficult to forecast workforce needs, assess skill gaps, or plan effectively for the future.
Additionally, achieving buy-in from senior leadership and fostering collaboration between HR and operational teams can be complex. Siloed approaches or a lack of appreciation for the value of workforce planning may hinder progress. Furthermore, balancing cost pressures with investing in workforce development and well-being requires careful prioritisation.
Over-reliance on independent contractors or contingent labour can also disrupt care continuity and lead to increased costs and loss of institutional knowledge. Providers must address these challenges with a proactive and flexible approach.
Auditing for Compliance with Outcome 2.8
According to the Evidence Mapping Framework and Strengthened Standards Provider Guidance, auditors will evaluate compliance through multiple categories of evidence.
This table summarises what evidence may be collected to assess conformance with Outcome 2.8
| Category | Details | Examples of Evidence |
|---|---|---|
| Documents and Records | Demonstrate the organisation’s workforce planning and management through clear policies, plans, and operational records. | Workforce strategy documents detailing the current workforce, skill mix, and future plans. Rosters showing alignment with care requirements. Training records tracking staff qualifications and ongoing development. Policies on recruitment, diversity, and contingency planning for shortages. |
| Management Practices | Show practical implementation of the workforce strategy and efforts to address shortages, support wellbeing, and promote diversity. | Contingency plans for workforce shortages, such as up-skilling and effective rostering solutions. Initiatives supporting staff wellbeing (e.g., mental health and wellbeing programs, feedback mechanisms). Evidence of diversity-focused hiring and psychological safety training. |
| Staff and Care Recipient Feedback | Show the perspectives of both staff and care recipients regarding workforce satisfaction, engagement, and care quality. | Staff surveys highlighting satisfaction, access to training, and perceptions of support. Care recipient surveys reflecting perceptions of care quality, continuity, and adequacy of staffing levels. Records showing how feedback was used to inform improvements. |
| Workforce Metrics | Provide data on staff numbers, qualifications, and competencies to demonstrate compliance with workforce planning requirements. | Metrics on staffing levels and ratios. Data on qualifications and mandatory training completion. Turnover and retention rates. Recruitment timelines and onboarding metrics. |
| Observations | Direct observation of care provision, staffing interactions, and roster implementation during the audit process. | Observations of rosters aligning with care needs. Staff engagement with care recipients. - Demonstration of team collaboration during service provision. |
Focusing on Workforce Development for Quality Care
Meeting the requirements of Outcome 2.8 provides a clear pathway for providers to focus efforts on building and maintaining this strong workforce. Outcome 2.8 highlights the importance of workforce development, retention, and well-being, ensuring that staff are not only qualified but also supported and empowered to provide the best care possible. This approach strengthens care provision, aligns with regulatory requirements, and prioritises the needs of both the workforce and the older people they serve.
References and Useful Resources
- Strategic workforce planning framework - NSW Public Service Commission
- National Nursing Workforce Strategy - Health Workforce Taskforce
- Strengthened Aged Care Quality Standards - Aged Care Quality and Safety Commission
- Strengthened Quality Standards Provider Guidance - Aged Care Quality and Safety Commission
- Evidence Mapping Framework - Aged Care Quality and Safety Commission
- Clinical Governance Standard (NSQHS Standards) - Australian Commission on Safety and Quality in Health Care
Author
Zoe Youl
Zoe Youl is a Critical Care Registered Nurse with over ten years of experience at Ausmed, currently as Head of Community. With expertise in critical care nursing, clinical governance, education and nursing professional development, she has built an in-depth understanding of the educational and regulatory needs of the Australian healthcare sector.
As the Accredited Provider Program Director (AP-PD) of the Ausmed Education Learning Centre, she maintains and applies accreditation frameworks in software and education. In 2024, Zoe lead the Ausmed Education Learning Centre to achieve Accreditation with Distinction for the fourth consecutive cycle with the American Nurses Credentialing Center’s (ANCC) Commission on Accreditation. The AELC is the only Australian provider of nursing continuing professional development to receive this prestigious recognition.
Zoe holds a Master's in Nursing Management and Leadership, and her professional interests focus on evaluating the translation of continuing professional development into practice to improve learner and healthcare consumer outcomes. From 2019-2022, Zoe provided an international perspective to the workgroup established to publish the fourth edition of Nursing Professional Development Scope & Standards of Practice. Zoe was invited to be a peer reviewer for the 6th edition of the Core Curriculum for Nursing Professional Development.



